Only 16% of residential care facilities are currently meeting the 200 direct care minutes requirement being introduced from October 2023 – 24 months from now – according to its latest Aged Care Financial Performance Survey for June 2021.
Just 11% of homes were meeting the future requirement for 40 minutes with an RN.
The data shows that of the 1,277 facilities surveyed (over 44% of the sector), direct care staffing hours have increased by an average of 0.7% in FY21 to 2.93 hours per resident per day.
Total care hours per resident per day have risen by 1.9% to 175.81 care minutes per resident per day.
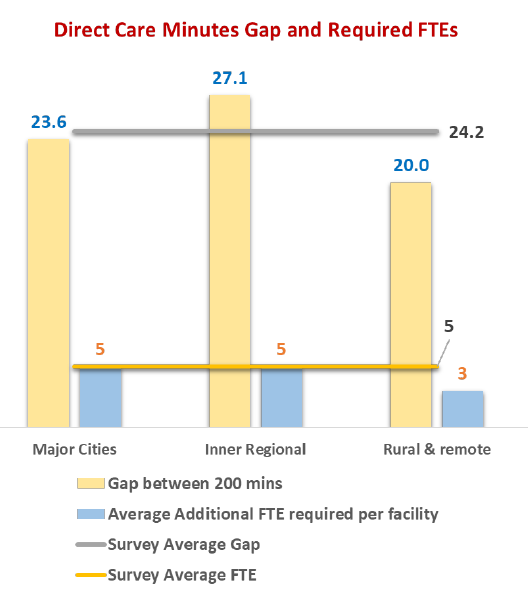
However, the minimum mandated minutes per resident per day (200 minutes for RN/EN/PCA staff) will require staffing to increase by an average of 24.19 minutes from the staffing levels for FY21.
 The Department of Health clarified earlier this year that the 200 minutes is an average, not a minimum requirement – but the impact will still be considerable, representing an overall increase of 13.8%, says StewartBrown.
The Department of Health clarified earlier this year that the 200 minutes is an average, not a minimum requirement – but the impact will still be considerable, representing an overall increase of 13.8%, says StewartBrown.
“To achieve this mandated level will require additional direct care staff to be employed. This will be a significant challenge for the sector, particularly in regional, rural and remote locations where registered nurse availability is at a premium,” their report states.
“Targeted initiatives designed to attract and retain staff will be the major strategic imperative in the coming years. Incentives which may include the provision of low cost accommodation and increased remuneration will require the funding and support from Government.”
In short, the Government will need to help providers, particularly those in regional, rural and remote areas, to foot the cost of meeting the new requirements – or the sector will be left facing a hefty bill.
While the care minute requirements are still two years away from being implemented, operators will also face increased scrutiny of staffing hours well before then.
Under the reforms, providers will be required to report on their care staffing hours on a quarterly basis and present residents and families with a monthly ‘care statement’ detailing the care they have received from July 2022 – less than eight months away.
This data will also be used to inform the star ratings being introduced in December 2022, which could impact on both occupancy and reputation of facilities.
With workforce already being labelled an “acute crisis” for the sector, will it prove to be ‘the straw that breaks the camel’s back’ for some operators?