Three years after the Government-run Oakden Older Persons Mental Health facility was shut down, prompting a string of State and national enquiries and ultimately a Royal Commission into the quality and safety of aged care in Australia, the Federal Government has announced – coinciding with World Elder Abuse Awareness day yesterday – that its Serious Incident Response Scheme (SIRS) will be in place in just over 12 months’ time.
The SIRS was first proposed by Kate Carnell AO and Professor Ron Paterson ONZM as part of a raft of measures outlined in their ‘Review of National Aged Care Quality Regulatory Processes Report’ which was announced in the wake of Oakden and presented to then-Aged Care Minister Ken Wyatt in October 2017.
Ahead of the establishment of the SIRS, the Government commissioned KPMG to look at incidents of abuse between aged care residents that are exempt from compulsory reporting (such as those where residents are living with dementia).
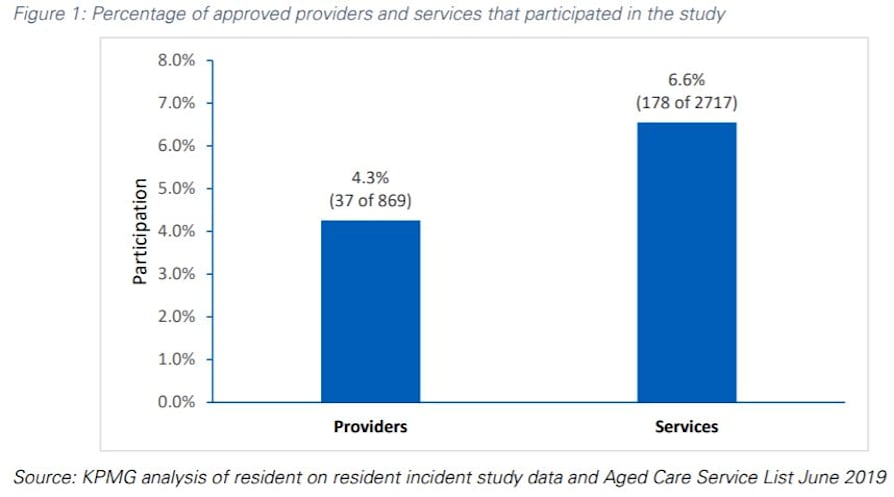
That study – released in November last year and updated this month – looked at a sample of 178 aged care services or just 6% of homes deemed to be “representative” of the sector including a cross-section for remoteness.
It identified a total of 1,714 incidents, extrapolating from that data that there must have been 52,600 unreported cases of abuse over 12 months at aged care homes nationally between residents – over 1,000 a week – with over 60% involving the “unreasonable use of force”.
Around 4.4% of cases were also deemed to involve “unlawful sexual contact”.
You must question if these numbers are satisfactory – 1,714 equates to just 3% of those 52,000 incidents.
The report also states that smaller homes and some States and Territories were under-represented in the findings. There is also no explanation of how these incidents were recorded, such as whether it was a tick in a box or a comment on a form.
KPMG acknowledges that its findings are subject to voluntary response bias – and it is not known whether non-participating services would have reported more or less incidents.
“Regardless, the study still provides the best available data on resident on resident incidents in residential aged care,” the report states.
Is that enough to set in play a system that will now always be there? See our weekly calculations below.
The scheme also represents yet more regulation for the sector – should operators be accepting it?
Under the new scheme, Aged Care Minister, Senator Richard Colbeck, says aged care providers will be required to inform the Aged Care Quality and Safety Commission (also established as part of the Carnell/Paterson recommendations) of allegations or suspicions of serious incidents, including neglect, psychological or emotional abuse and inappropriate physical or chemical restraints.
Minister Colbeck also revealed that a similar scheme is on the cards for home and community aged care, with part of the funding to go towards a prevalence and feasibility study to inform future Government decisions on the potential introduction of a SIRS for aged care services in the home.
The new reporting requirements will significantly increase the regulatory powers of the Quality and Safety Commission, which will receive the incident reports, be able to conduct its own investigations of such incidents and take regulatory action where needed.
Critically, it will get rid of the current exemption on the reporting of resident-on-resident incidents where the perpetrator has a cognitive impairment such as dementia and the provider take steps to manage their behaviour within 24 hours.
Based on the figures above, this theoretically means up to 1,000 new investigations a week the sector will need to respond and cooperate with (or 200 per working day).
Even if they only investigate one-quarter of the cases, that is 50 a day. Based on our calculations, if each investigation requires five hours of a senior manager, 50 investigations will require 1,000 hours a week – before you even throw in the costs of running the SIRS.
This investment in time is justifiable if the ‘problem’ is systemic, but is it?
Is the sample big enough and truly representative, or simply the best KPMG could get and therefore acceptable?
Will the sector just accept this and a burdensome system, which once started will unlikely be withdrawn?
“We understand there is still much work to do,” Minister Colbeck said. “Improving aged care for senior Australians continues to be one of the Morrison Government’s key priorities.”
As Maroba Aged Care CEO Viv Allanson perfectly summed up last week, operators have already faced a “perfect storm” of poor funding, new service models and Quality Standards, the impact of the pandemic and the overall global financial situation, and the extra costs for staff and PPE.
How many operators will be tempted to throw in the towel?