The latest StewartBrown Aged Care Financial Performance Survey has again delivered improved results for residential aged care providers – but also hinted at the increasing pressure that operators will face in the leadup to the mandated requirement for 215 direct care minutes per resident in October.
As we report in this issue, the latest StewartBrown results for the six months to 31 December 2023 show that residential aged care operators continue to deliver a surplus on care – though they are still haemorrhaging cash on accommodation and daily living expenses.
These losses should be addressed by the Government’s response to the Aged Care Taskforce’s recommendations.
What won’t be dealt with is the real pain point facing providers: workforce, specifically the shortage of Registered Nurses (RNs) and the cost to fill the gap.
The StewartBrown report notes providers are still falling short on the requirement for 40 direct care minutes with an RN despite spending up big on agency staff – the use of agency RNs remains around 10% of total RN usage even after an extensive recruitment drive over the last year.
This comes at a significant cost – the average agency RN hourly rate is $124.44 per hour – see below.

Image credit: StewartBrown
StewartBrown says it would cost providers another $5.75 per bed day to bridge the gap between the current RN minutes and the 40 minute target – currently at 2.77 minutes.
215 care minutes commences in October
This gap is about to become wider.
Residential aged care operators are now just six months away from the increase in the mandated direct care minutes to 215 minutes per resident per day – including 44 minutes with an RN.
Of course, not all providers are meeting the targets – and the regulator has openly stated that it isn’t pursuing operators that are under the requirements unless they deem there is a serious risk to residents.
But while these operators may be saving on labour costs, they do risk being penalised on staffing for their star rating – and who wants to put Mum or Dad into a two- or three-star rated facility?
All of this adds up to additional staffing costs for providers – and that is without even taking the Stage 3 Fair Work Commission ruling into account (StewartBrown forecasts that this will increase staff costs by another $13 per bed day excluding historical leave entitlement – see below).
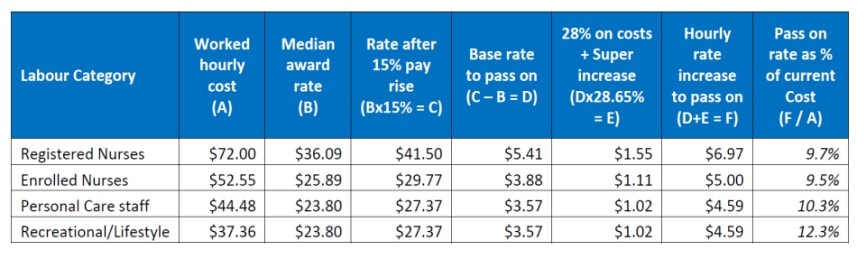
Image credit: StewartBrown
In Parliament this week, Minister for Aged Care Anika Wells revealed that the sector has now reached 24/7 RN coverage in aged care 98.79% of the time – with 90.02% of aged care homes having an RN on site 24/7.
“That is an achievement that those opposite didn’t even dream of attempting in Government, let alone legislating for and let alone budgeting for,” she stated.
“Under the Albanese Government, older people are receiving an additional 2.16 million minutes of care every single day.”
While this is an achievement, can the Government also deliver the higher subsidies that will be required for providers to meet these increasing staff costs?
Will this be the straw that breaks the back for some operators?










