The 3 key attributes of the ACFI coordinator in an AN-ACC world
By: Andrew Farmer (pictured below), CEO, Mirus Australia In May this year, the Government announced the proposed timing for the launch of AN-ACC, together with the details for funding and the shadow assessment process. Since then, the Department has...

By: Andrew Farmer (pictured below), CEO, Mirus Australia

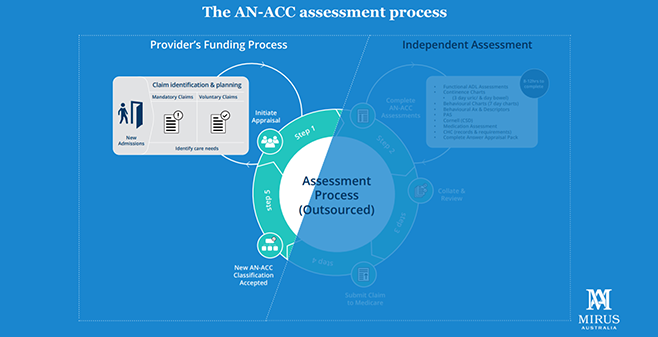
In May this year, the Government announced the proposed timing for the launch of AN-ACC, together with the details for funding and the shadow assessment process. Since then, the Department has released several updates with new information and thousands of shadow assessments have been completed. I’ve spent time with over a dozen CEOs in recent weeks to discuss how they’re preparing for the transition. One of the common questions I hear is, “How will AN-ACC change my current ACFI resources?” It’s an important question and it’s possible that the pending funding change might already be having an impact on your team. To understand what will be required, we started looking at the role of current ACFI resources and how ACFI roles in our industry add value to organisations. We also looked at the AN-ACC assessment process and the implications for existing roles. We can summarise the current ACFI process into five steps from identification and initiating the appraisal to the acceptance of the new ACFI classification. This process has been fine-tuned over the last 10 years and will be very familiar to all who are close to ACFI. There are challenges in this process, particularly the bottleneck caused at Step 2 (pictured above), where significant documentation needs to be created. The recent shadow assessments have given us some insight to what an external assessment process might look and feel like. What we do know is that the internal requirement for assessment and documentation will be significantly reduced. In the diagram below, we illustrate this by removing Steps 2-4. It would be oversimplifying the change to suggest that all of the work will be removed. High performing providers will still have the capability to assess and understand any potential changes to AN-ACC so that the outcome of the assessment/re-assessment process is more predictable.
So what does this mean for future AN-ACC resourcing?
Through our discussions with providers and our own history working with ACFI teams across the sector, we have defined three key attributes of a great ACFI resource. We’ve then used them to characterize the attributes of a ‘Clinical Funding Advocate’ (CFA), a role that would enable the transition from ACFI to AN-ACC. The three attributes are Business Management/Analytics, Clinical Management and Resource Management. These attributes are described in more detail below in terms of how they add value now and how that may change in the ANACC world.
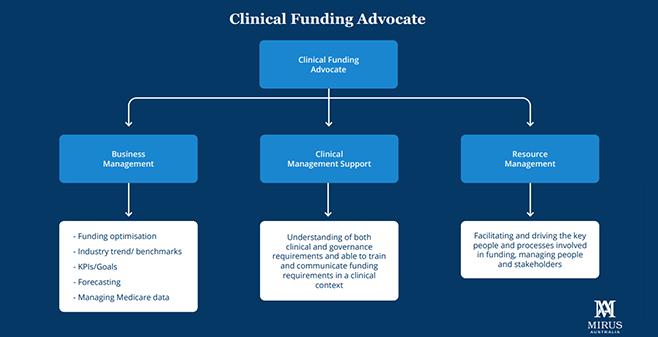
1. Business Management/ Analytics (100% – 120% remaining)
The CFA has a core responsibility to be on top of the data. Clinical funding data produces a wealth of insight into the funding performance of clinical operations. As the funding model derives most of the income for a RAC, this role is a significant driver of the income for the business. While ADS is commonly used as a KPI, it is an average of several underlying metrics. The most competent funding managers are working with Finance and Operations managers to analyse several benchmarks, metrics and ratios to determine the performance of their funding processes. As we transition to AN-ACC, the proportion of funding from the new model will be just as critical, and therefore the ability to analyse and act on the insight from the data will be similar. Furthermore, linking AN-ACC data to minimum care requirements for each classification could pave the way for the most data driven funding, rostering, admissions forecasting and modelling in real time that the industry has ever been able to achieve. Those with the systems and analytics to manage these data sets will be ahead of the curve and the most in control of their sustainable profitability.
2. Clinical Management (25% – 50% remaining)
Many of those that find their way to funding roles have come from a clinical background. This gives them the ability to translate the funding requirements into clinical terms. As much as care is the primary focus of all aged care businesses, the importance of translating care information into funding information is critical to fund the care being provided. Great clinical management therefore depends on the knowledge and experience of how to support the funding processes with the required clinical evidence. In the new AN-ACC world, a great deal of this part of the process will be “outsourced” in the new external assessment process. The most important change in this aspect is that the ‘provider becomes the validator’. The provider must know the rules and requirements equally well to be sure that a fair and accurate result is achieved in all cases (and in some cases, avoid the cost of the re-assessment if it is unsuccessful). This means that while the volume of assessment and charting documentation required to support funding may all but disappear, the specialised knowledge and advocacy of the process will need to remain with a few champions and/or a trusted business consulting partner. Much of the savings may be in the part-time ACFI resource that is assigned in the facilities where these valuable and typically experienced clinical resources will easily find redeployment.
3. Resource Management (50% – 75% remaining)
The third critical element that exists in funding advocates today is the ability to get the process done. In our experience, there are almost as many models for ACFI management as there are providers. These models have evolved over time based on changing structures, acquisitions and changing personnel at all levels of the business. In many cases, we see a variation on the centralized or decentralized ACFI resources, but the number and quality and dedicated focus (not hybrid roles and responsibilities) varies considerably. The highest performing in ACFI have invested heavily in knowledge and resource, and they reap the benefits from higher funding because ACFI is a model that rewards high levels of activity and timeliness. While it is true that the volume of work (particularly clinical work) will be reduced due to the external assessment process, the number of moving parts will still be many. These will include the quality of the data in care systems, analysis of funding data and the identification of reassessments, the assessment of new residents and the process of managing the external assessors (as some providers have learned through the shadow assessment process). All of these changes are happening in the context of the broader aged care reforms, and it will be difficult to move forward by focusing on one element and ignoring others. The new star ratings will depend in part on care minutes, which will in turn depend on AN-ACC classifications (for case mix adjusted care minute targets). Both items will depend on the changing resident mix affected by Admissions. In summary, there will be significant changes to your internal process and resources with the change from the ACFI funding model to AN-ACC, but not everything will change. The ‘Clinical Funding Advocate’ role will remain. Will there be opportunities to bring this role closer to Quality or closer to the Finance team? The answer to that will depend on your organizational structure now and where you want it to be in the future.
Further resources:
- Mirus AN-ACC Essentials training
- Mirus ACFI and AN-ACC calculator
- Mirus ACFI to AN-ACC Pathway (MAAP), a diagnostic to map your transition progress
- Mirus AN-ACC Resource Hub with news, tools and services
About Mirus Australia
At Mirus, we help you take control of your aged care business. Our tools and services give you immediate insight into your biggest challenges: workforce, funding, compliance, costs, and customers. Find out what’s working well and what isn’t in real-time. Spend less time with paperwork and systems and more time planning for profitability and growth. Our solutions have been designed exclusively with your success in mind. Everything we do is for aged care.






